Genomics of Cancer and Targeted Therapies
Introduction
Genomics of Cancer and Targeted Therapies is an IFOM research program coordinated by Alberto Bardelli, dedicated to studying genetic differences in tumors and the therapeutic opportunities stemming from this complexity.
As historically significant as the sequencing of the human genome, the effort to sequence cancer genomes has reached an advanced stage, uncovering pivotal insights in modern medicine.
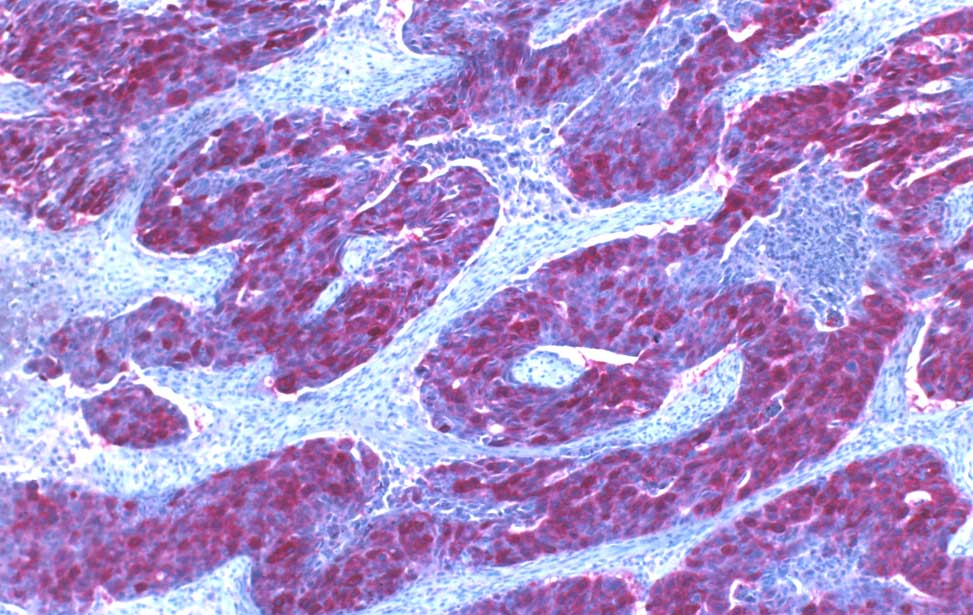
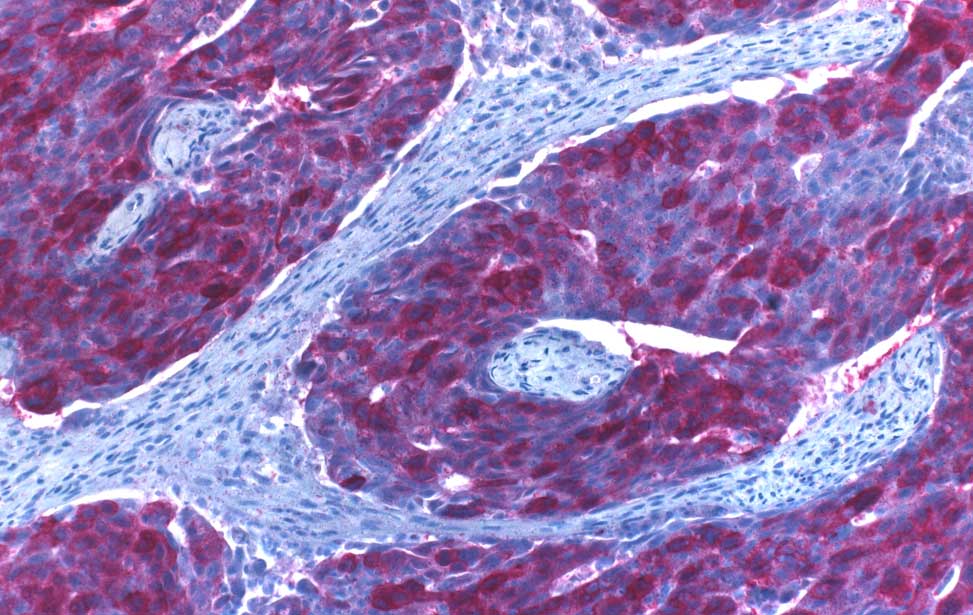
It is now well-established that the genes most frequently implicated in cancer—those that, when mutated, strongly drive cells toward malignant transformation—are relatively few. However, there are also genes that, although rarely mutated, can nonetheless drive tumor growth. Beyond this complexity, the variety of ways in which distinct mutations combine with one another and with normal genomic background contributes to the emergence of heterogeneous tumors, both within the same disease type (e.g., colorectal cancers are not all alike) and within the same individual (even within the same tumor mass).
The clinical implications of this heterogeneity are profound.
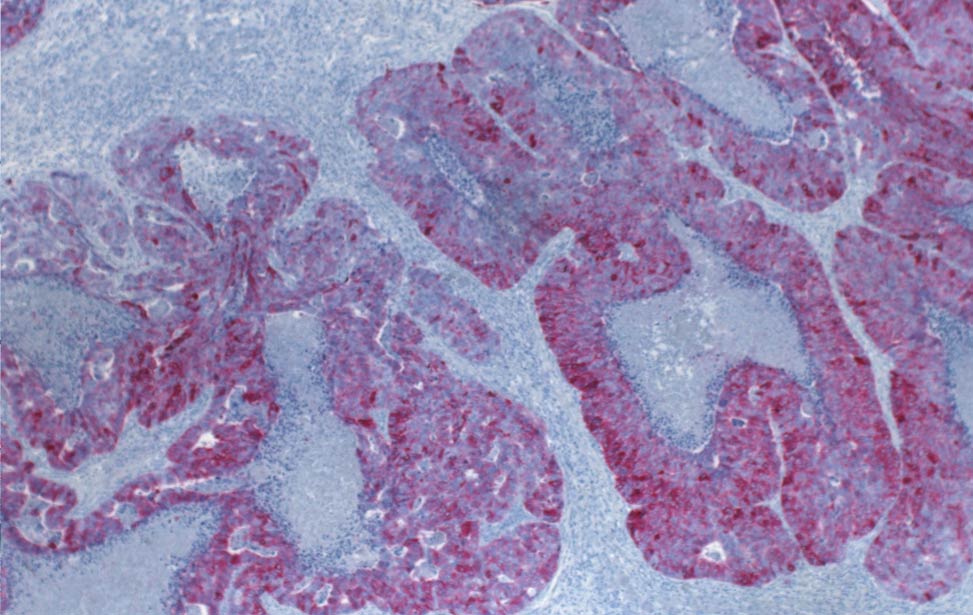
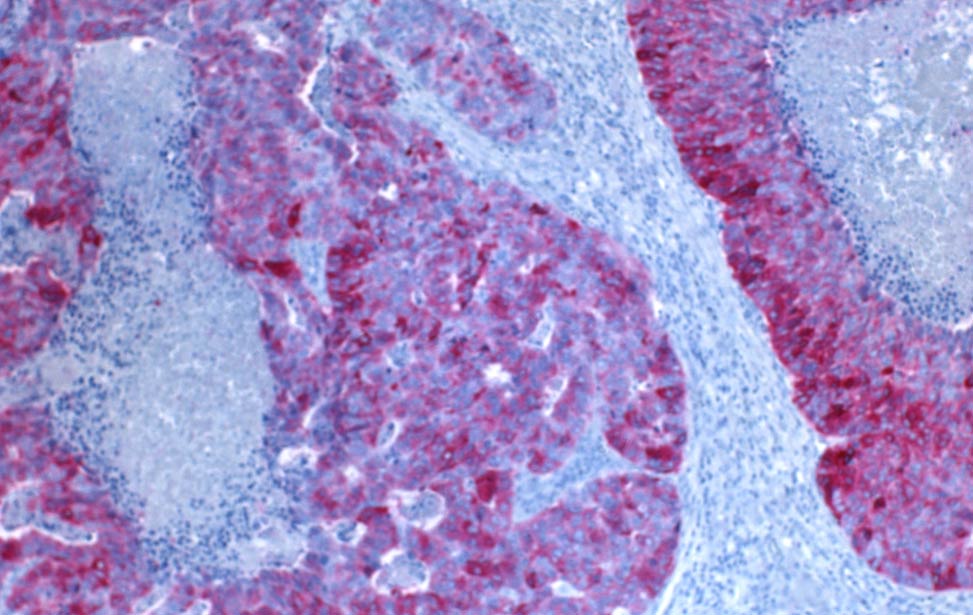
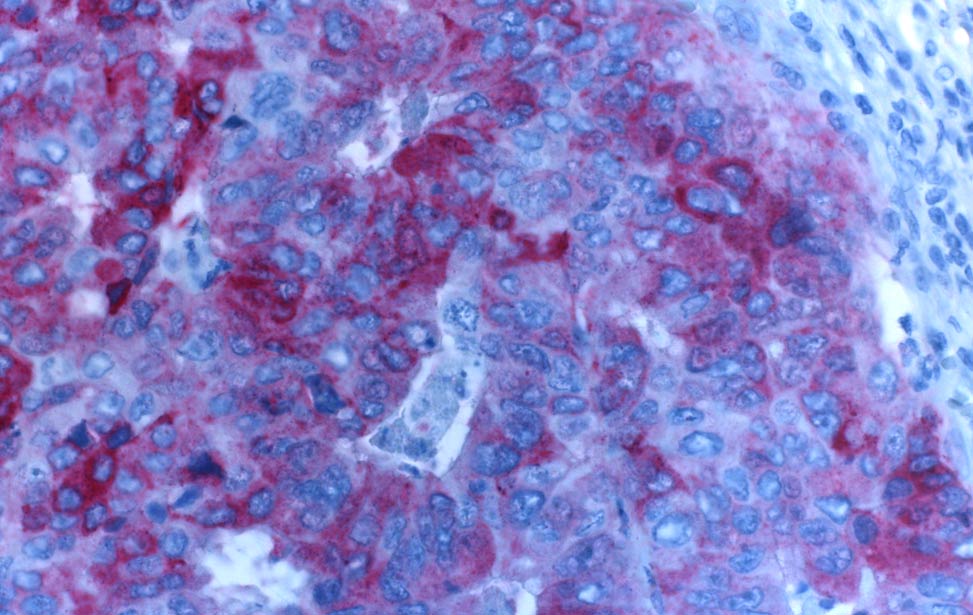
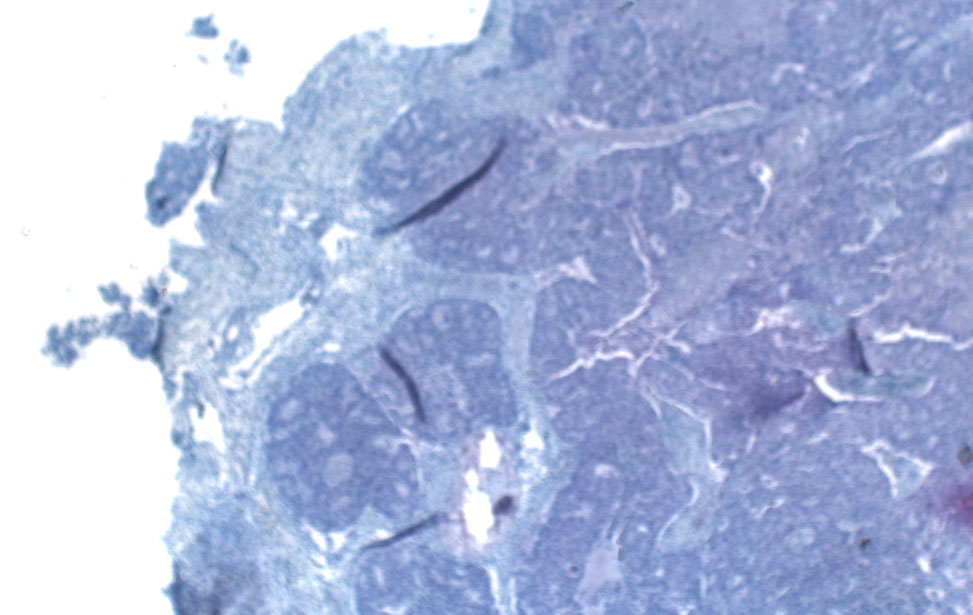
Tumors that appear similar under histological examination of diseased tissue and are treated similarly may, in fact, represent molecularly distinct entities, responding differently to therapies and exhibiting divergent clinical outcomes.
In an era increasingly oriented toward precision medicine, the genetic profile of a tumor has become an essential and strategic element for personalized patient care.
For over 15 years, Alberto Bardelli and his team, through its Genomics of Cancer and Targeted Therapies based at IFOM and the University of Turin, have been focusing on the genomic study of solid tumors.
Specifically, colorectal cancer, one of the most prevalent and lethal cancers in Italy and worldwide, lies at the heart of the laboratory’s research, aiming to:
- Analyze the genetic profile of tumor cells;
- Monitor their evolution throughout disease progression and treatment;
- Understand how tumor genomes influence response to pharmacological treatments, guiding optimal therapeutic choices for individual patients;
- Investigate the connection between DNA mutations, the generation of neoantigens (altered proteins resulting from mutations), and tumor recognition by the immune system, with the goal of understanding if and how this interaction can be modulated.
Biological Scope
The IFOM Genomics of Cancer and Targeted Therapies program focuses on solid tumors, particularly colorectal cancers, to determine how their genetic landscapes influence tumor responses to targeted treatments, thereby improving the personalization of care.
Cancer is indeed a genomic disease.
Within the genome, mutations accumulate over a person’s lifetime, transforming normal cells into malignant ones. It is also in the genome—within the specific combination of genetic alterations developed during tumor transformation and progression—that lies the explanation for the diversity between two distinct types of cancer, as well as between two malignant cells within the same tumor, following uncontrolled cellular multiplication that increases its mass.
In the tumor genome, we find critical clues to better understand cancer biology, define precise diagnostic markers for different cancer forms, predict clinical progression, and identify specific targets for designing tailored drugs that act in a targeted and not indiscriminate manner.
Several innovative drugs have demonstrated the potential to radically change the therapeutic landscape for specific cancer types, including colorectal cancer.
However, the success of this approach depends not only on the presence of its target in the tumor but also on the genetic context in which it operates. These contexts can foster resistance to therapy, either primary or acquired.
An emblematic example is drugs targeting the epidermal growth factor receptor (EGFR), widely expressed in colorectal cancer cells. Alberto Bardelli’s group was among the first to study the genome role in determining response to anti-EGFR therapy.
In these cancers, as in many others, EGFR activates signaling cascades that drive malignant cells to proliferate uncontrollably, form tumor-specific blood vessels, and invade other organs and tissues.
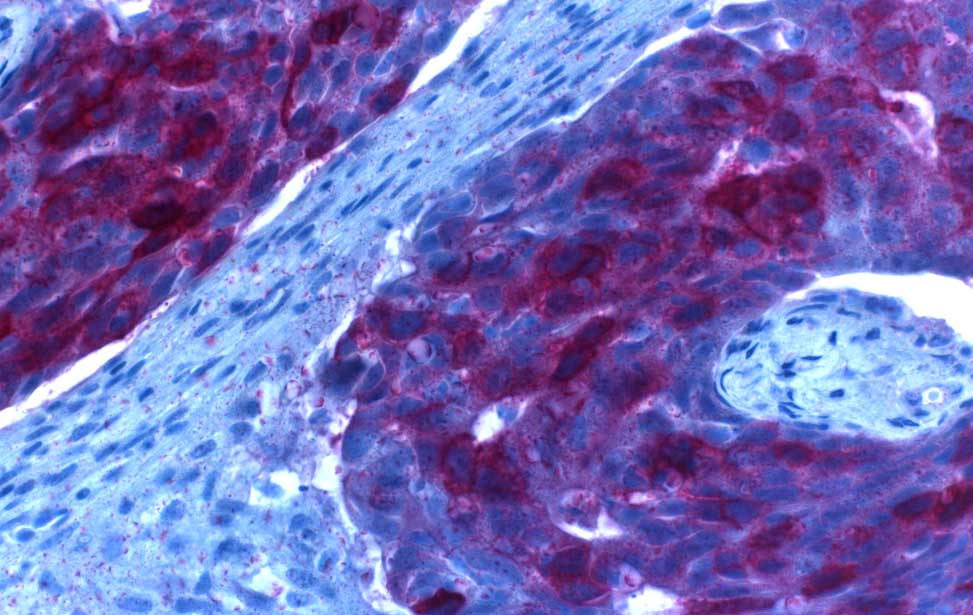
Anti-EGFR therapies, frequently used in metastatic colorectal cancers, can interrupt these signals and halt tumor growth. However, as EGFR represents just one component of the complex machinery underlying the malignancy of these tumors, other downstream genes—disrupted by mutations—often bypass EGFR inhibition, precluding treatment benefits. Resistance mutations, initially absent or present in only a minimal proportion of heterogeneous cells, may also emerge under therapeutic pressure, leading to resistance after an initial benefit. Even in the absence of acquired mutations, tumor cells can enter a quiescent state (that we and others defined as persister cells), enabling survival during treatment by dynamically modulating specific gene expression patterns. Studies on EGFR have shown that the same signaling pathway may mediate drug sensitivity or resistance differently across patients—or even among tumor cells within the same patient.
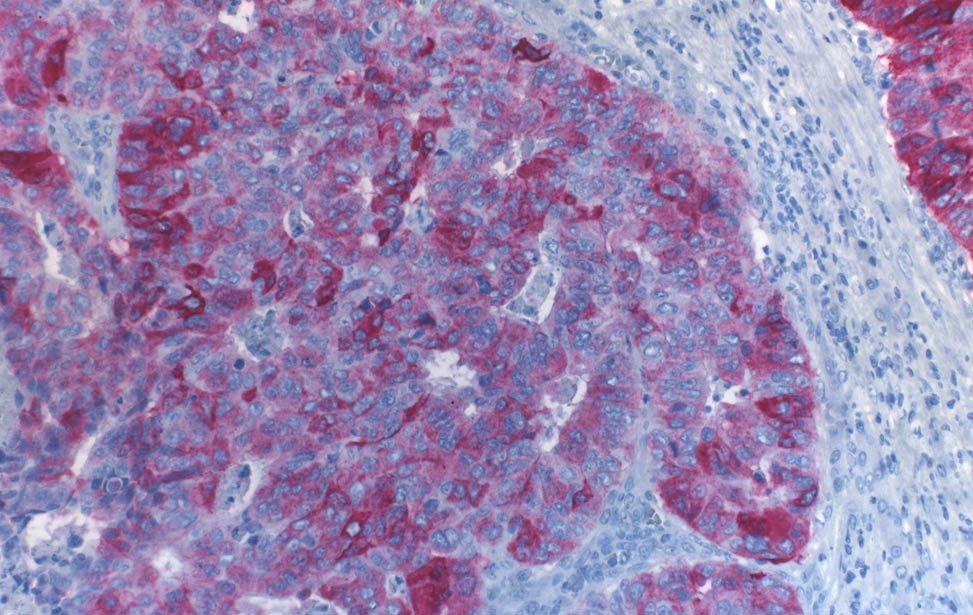
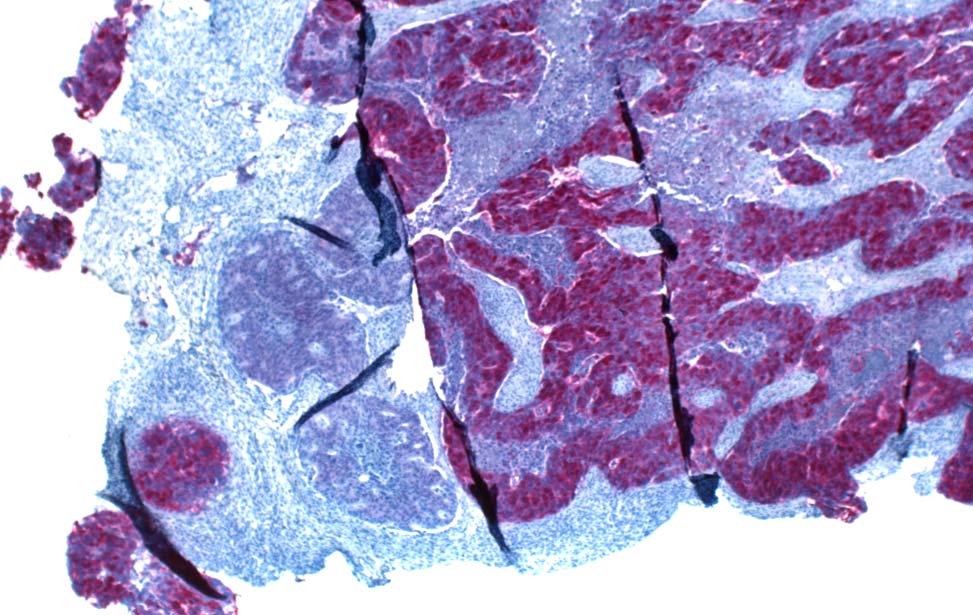
The immune system’s surveillance against tumor cells can similarly be influenced by the tumor genetic features, another focus of the laboratory’s research. A small subset of colorectal cancers (immune-hot MSI tumors) arises and progresses due to congenital or acquired defects in DNA damage repair mechanisms. These cells, unable to preserve their genome, acquire a high mutation load, generating altered proteins (neoantigens) that enable clear immune recognition of their abnormal nature. Once engaged, the immune system becomes a highly effective antitumor weapon.
Program Goals
Many insights into the sensitivity and resistance of metastatic colorectal tumors to molecularly targeted drugs, such as EGFR inhibitors (and later HER2 and other targets), have emerged from studies conducted by Alberto Bardelli’s team.
However, much remains to be investigated to overcome the challenges faced by targeted therapies and to optimize treatment strategies in solid tumors.
In addition to analyzing tumor genetic landscapes and identifying pharmacogenomic correlations—linking drug activity profiles to the genetic features of malignant cells—the IFOM program also explores the relationship between the genome and other omics (e.g., transcriptomics, epigenomics, proteomics, metabolomics). This integrative approach delves into the molecular basis of cancer and resistance to treatments, with a particular focus on emergence mechanisms of resistance.
The importance of identifying mechanisms of drug resistance lies indeed in the potential to forestall them, for example, through co-administration of molecules (dual blockade). One case is HER2-targeted therapy, which requires this approach to induce tumor regression in HER2-dependent colorectal cancers. Another is anti-BRAF therapy, for which Bardelli’s team elucidated resistance mechanisms, demonstrating the need of dual blockade to achieve a therapeutic response.
Ultimately, the program aims to provide effective tools for identifying molecular vulnerabilities in solid tumors—primarily colorectal—and determining the optimal sequence or combination of therapies based on genetic characteristics, thereby challenging current therapeutic limitations.
Approaches
The research unit employs diverse molecular genetics and cellular biology techniques in its studies. Consistent with the IFOM mission to translate scientific progress into tangible benefits for patients with cancer, the group is actively involved in numerous international clinical studies, contributing genomic and omics analyses of patient samples to generate new therapeutic hypotheses.
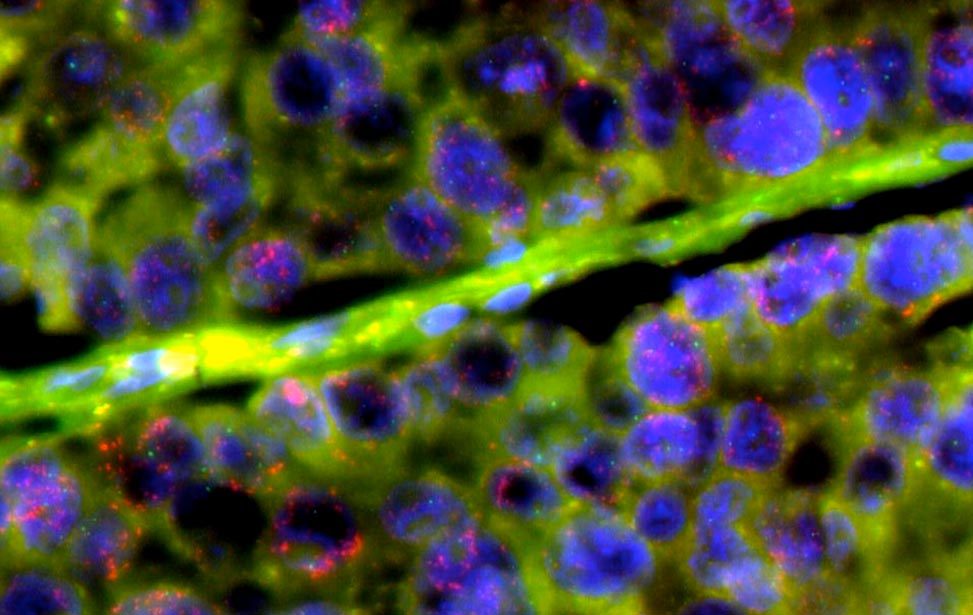
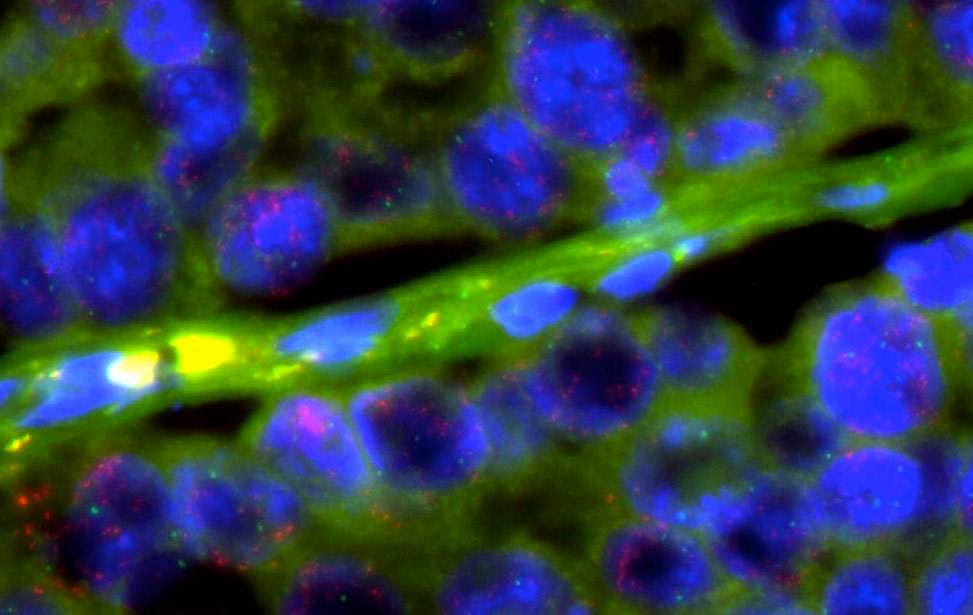
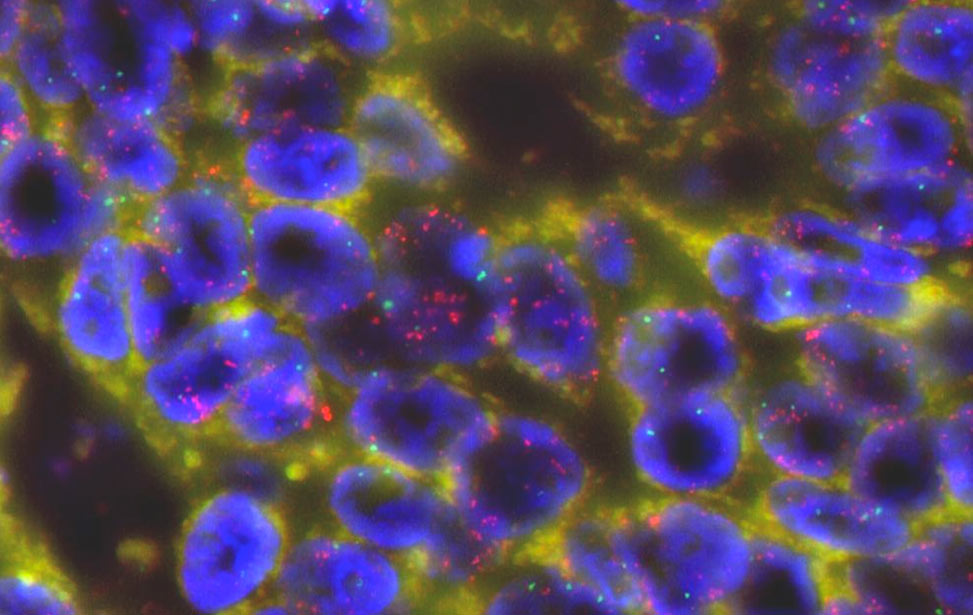
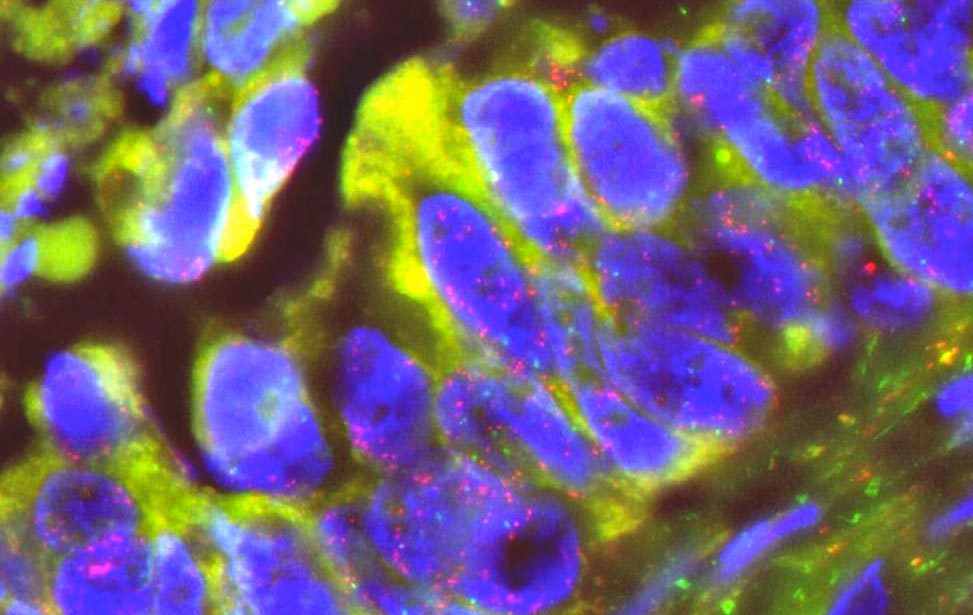
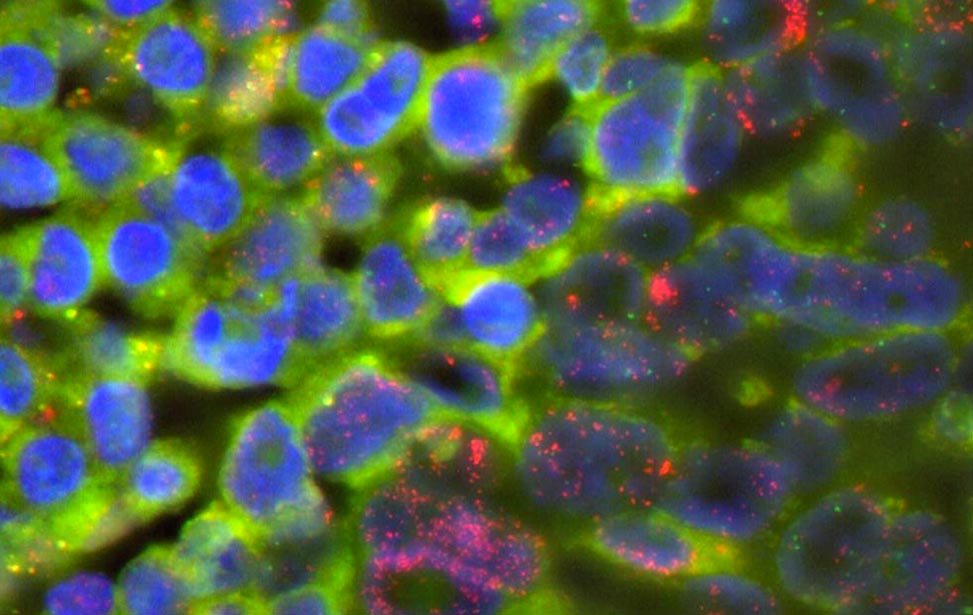
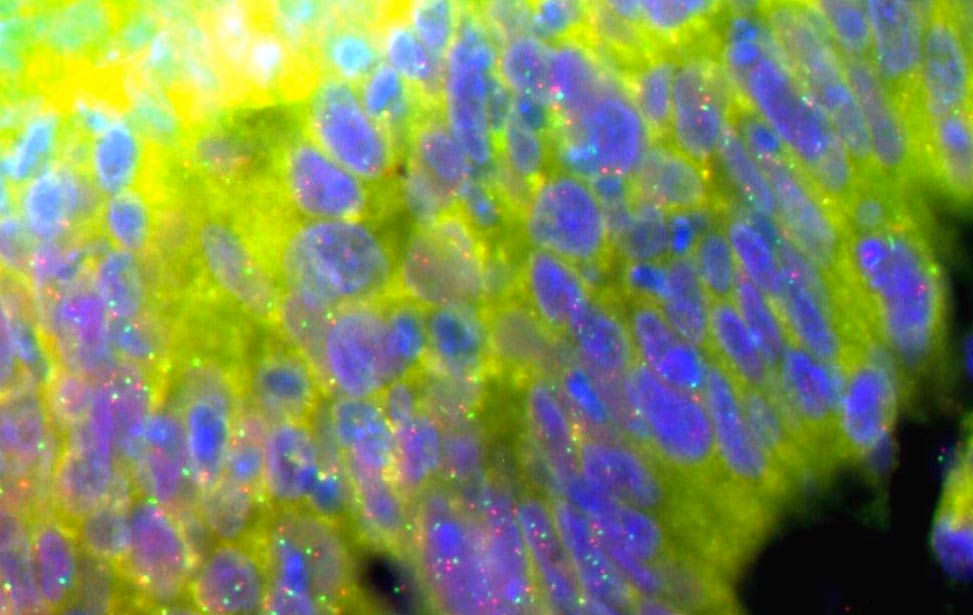
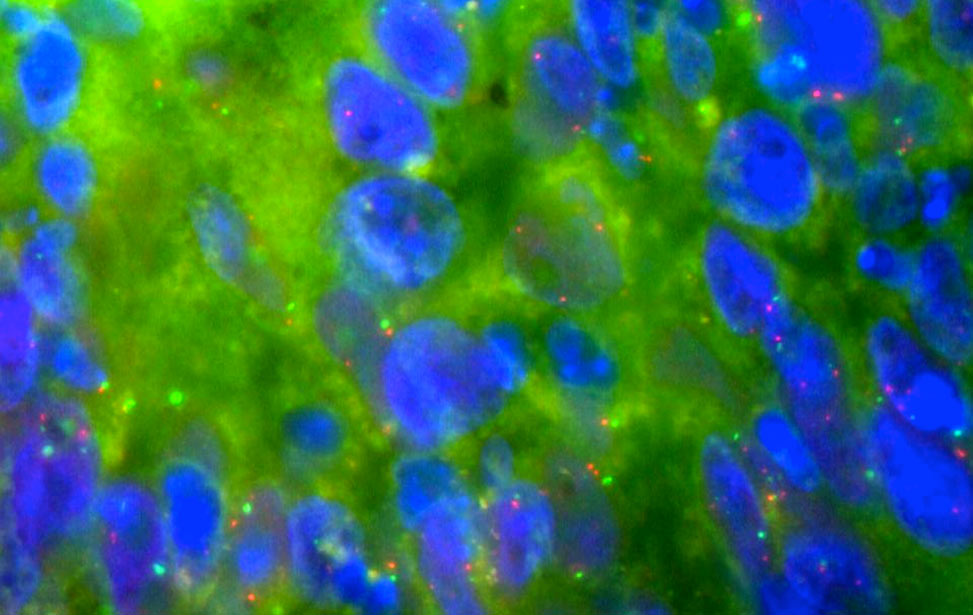
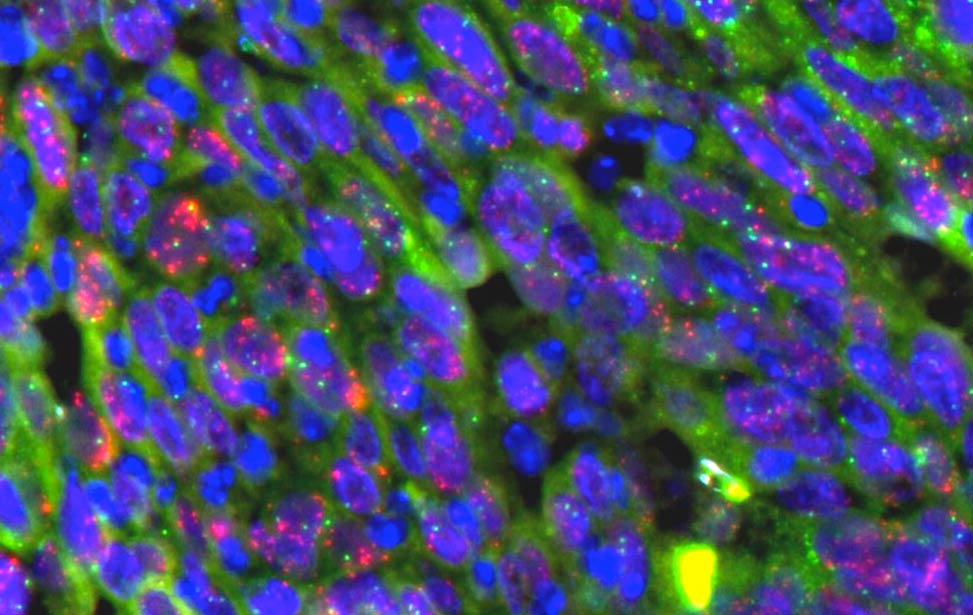
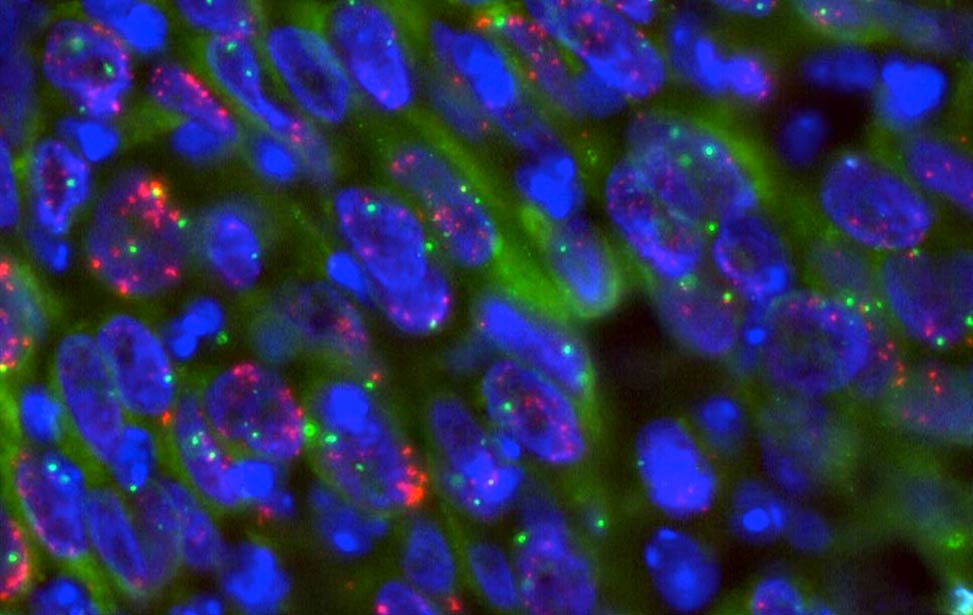
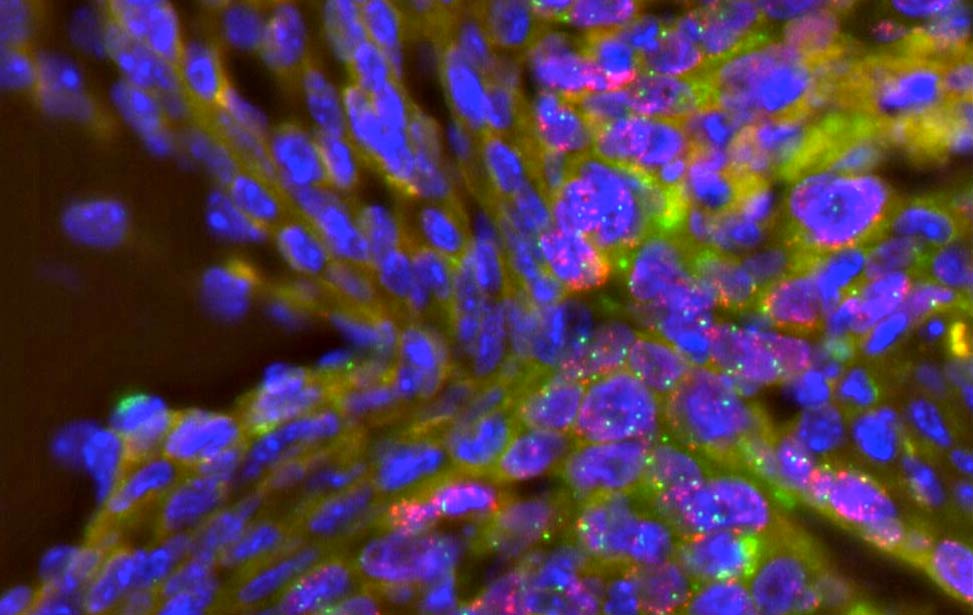
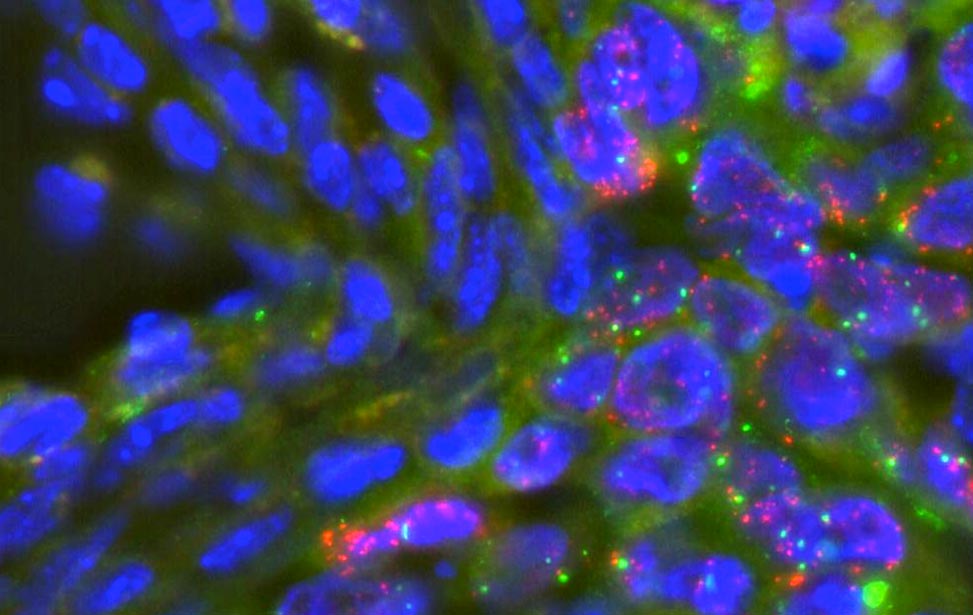
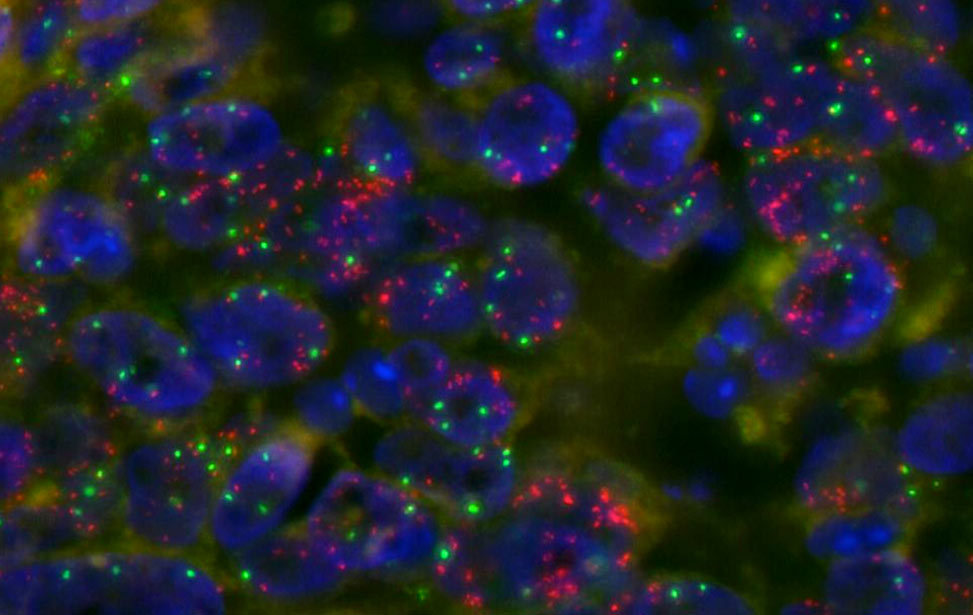
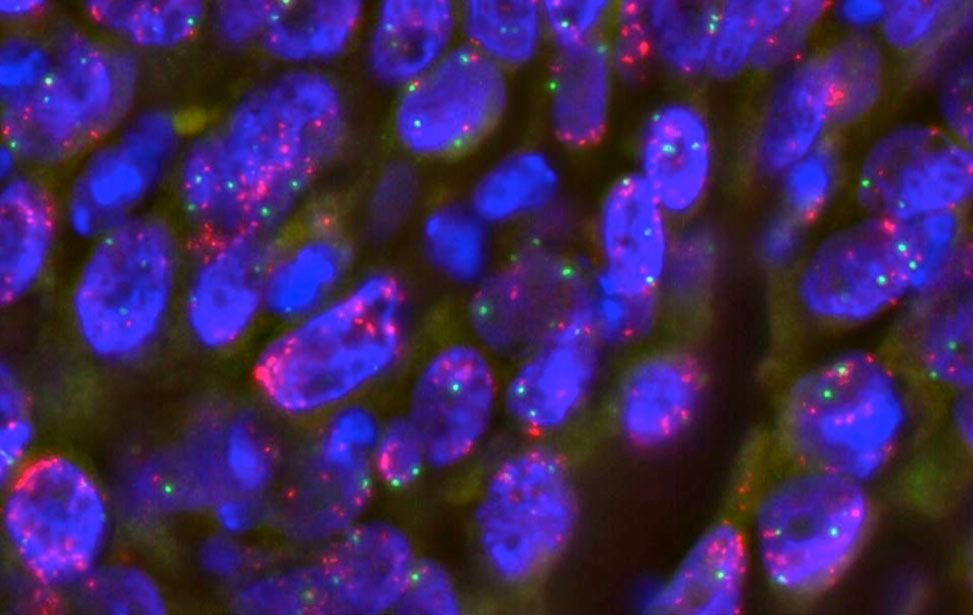
Cancer cell models that replicate the molecular traits of tumors of interest, derived directly from human samples, enable detailed studies of tumor biology—such as proliferation signals—and evaluation of anticancer therapies, including targeted treatments and immunotherapies. These models effectively create patient-specific avatars for testing therapeutic options.
Patient genetic and molecular profiles are reconstructed using cutting-edge genome analysis technologies, particularly next-generation sequencing (NGS), which can sequence entire genomes rapidly.
Previously reliant on invasive biopsies, genomic studies can now leverage blood (and other easily accessible fluids like urine) for equivalent insights. Bardelli’s team pioneered liquid biopsy development, a non-invasive method using blood to analyze tumor-released DNA fragments, simplifying and enhancing monitoring of genetic profiles and disease progression.
This research program’s hallmark is its clinical impact, with genomic and omics studies directly influencing patient care. Multidisciplinary collaboration between biologists, geneticists, and clinicians ensures that insights are swiftly translated into clinical practice.
Impact on Diagnosis, Prevention, and Treatment
The results of the Genomics of Cancer and Targeted Therapies group have revealed that even tumors with similar origins and histological features (morphology, pathological characteristics, etc.) can harbor significant molecular heterogeneity. This heterogeneity translates into variations in disease outcomes and differing responses to pharmacological treatments, including targeted drugs, from patient to patient.
The ability to develop treatment strategies that precisely address the biological characteristics of tumors, therefore, relies on the findings of genomic and molecular studies, which are a key focus of Alberto Bardelli’s group.
An paradigmatic example of what is now considered a major step forward in personalized medicine is indeed the treatment of colorectal cancer.
Fifteen years ago, patients with metastatic colorectal cancer were treated with EGFR-targeted drugs, considered among the most effective therapies at the time. However, only 10–20% of patients benefitted from these treatments. Thanks to the studies conducted by Alberto Bardelli’s group, we now understand why.
A significant portion of colorectal cancers harbor molecular alterations (most commonly mutations in KRAS and BRAF) that prevent response to anti-EGFR therapies. This discovery, which has made history in oncology by transforming clinical practice, enabled better patient selection for this type of treatment, increasing the likelihood of response in eligible patients and sparing others from unnecessary toxicity due to predictable resistance.
Furthermore, Bardelli’s work demonstrated that, when resistant malignant cells emerge following treatment—due to the selection of resistance mutations—the tumor ceases to respond to therapy as it evades the drug blockade. Researchers monitored these mutations non-invasively in patient blood samples after treatment, uncovering their dynamic nature. Specifically, resistance mutations, after some time, can be counter-selected by new therapies, eventually disappearing and rendering the tumor sensitive again to a rechallenge with targeted drugs.
In the patients' interest, this observation was promptly translated into a clinical study demonstrating that liquid biopsy can be used to determine the optimal timing for an anti-EGFR rechallenge.
Similarly, liquid biopsy has been applied to other important recent clinical studies by the group on colorectal cancer. For instance, it has been used to monitor the drug-induced transformation of immune-cold tumors into hot tumors, informing the possibility of administering immunotherapy in initially non-responsive cases (most colorectal cancers are not sensitive to immunotherapy). Liquid biopsy has also been employed to detect residual tumor cells not visible through conventional imaging after surgery, enabling prediction of recurrence risk and pharmacological interventions to modulate the intensity of post-surgical (adjuvant) chemotherapy.
These and other insights generated through the IFOM Genomics of Cancer and Targeted Therapies research program, coordinated by Alberto Bardelli, aim to significantly improve the diagnosis and treatment of patients with solid tumors by translating research findings into clinical practice.